When a loved one is diagnosed with Alzheimer’s and other dementias, families face a long and emotional journey. Understanding the stages of dementia before death can help them navigate the challenges.
As Alzheimer’s disease progresses, it gradually affects memory, reasoning, and behavior. Each level brings challenges that are unique to every person. Understanding the stages of dementia before death can help caregivers prepare, adapt, and provide compassionate care.
While every individual’s experience is unique, healthcare providers often use the Functional Assessment Staging measure and the seven-stage model of Alzheimer’s progression developed by Dr. Barry Reisberg, known as the Global Deterioration Scale (GDS).
The stages of dementia before death
Stage 1: No noticeable impairment
In the earliest stage, dementia may be barely obvious. A person can function normally in daily life, and any memory lapses can appear typical of aging. Families and friends may not notice any signs right away.
Support is not usually needed here, but as signs begin to appear, a professional assessment can differentiate between mere forgetfulness or dementia. If a diagnosis is made, it is a good time for families to begin learning all that they can about the disease and measures to take. Some forms of memory loss can be treated or even reversed. Even if the diagnosis is Alzheimer’s or another form of dementia, professionals can recommend steps to improve quality of life.
Stage 2: Very mild cognitive decline
This stage can resemble having “senior moments” such as occasionally misplacing objects or forgetting a familiar word. Because symptoms at this stage are subtle, they may continue to go unnoticed by others.
Brain-healthy activities such as reading, doing puzzles, and having regular exercise may help maintain cognitive function or forestall further decline.
Stage 3: Mild cognitive impairment
At this stage, memory lapses become more apparent. A person may have trouble recalling names, organizing daily tasks, or following conversations. Friends, coworkers, or family might notice the changes, which can cause embarrassment or frustration for the individual.
This is the time to begin active support, such as helping with organization and reminders. Families should also initiate conversations about future care preferences and legal planning, since independence will gradually diminish.
Stage 4: Moderate cognitive decline
 At this stage, dementia becomes more evident in daily life. A person may struggle with managing finances, traveling to unfamiliar places, or remembering details of their past. Their personality may change at this point, and they may withdraw from social situations.
At this stage, dementia becomes more evident in daily life. A person may struggle with managing finances, traveling to unfamiliar places, or remembering details of their past. Their personality may change at this point, and they may withdraw from social situations.
Caregivers can establish predictable routines to help reduce confusion and offer emotional support when frustration or sadness arises. If you have not already, begin planning now. Finalizing legal and financial matters now can help avoid complications later.
Stage 5: Moderately severe cognitive decline
In this stage, the patient will no longer be able to be able to manage their personal affairs independently. They may forget familiar details such as their address, phone number, or even the names of close family members. Assistance with dressing, meal preparation, and personal care becomes necessary.
Caregivers should prioritize their loved one’s safety, ensure proper nutrition, and seek outside support. Compassionate, hands-on help is essential, from non-medical home care to home health care. Structured activities like listening to music or looking at family photos can provide comfort and preserve emotional connections.
Caregivers should also take care of their own needs, including sleep, healthy eating, maintaining social connections, and seek outside assistance as needed.
Related: Caregiver Stress – Is It Time for Memory Care?
Stage 6: Severe cognitive decline
At this stage, memory loss is profound, and a patient may not recognize their spouse, children, or lifelong friends. Behavioral changes such as agitation, wandering, or paranoia are common. Physical challenges such as difficulty walking, incontinence, or trouble swallowing begin to emerge.
Caregiving becomes even more intense. The patient needs assistance for nearly every aspect of daily life, from bathing and toileting to eating. Professional care, whether in-home or through assisted living, is often necessary. Emotional support for caregivers themselves is equally important, as stress and burnout can be overwhelming. Knowing some strategies on caregiving for dementia patients can help both caregiver and their loved one.
Stage 7: Very severe cognitive decline
The final stage of dementia is marked by the loss of verbal communication, mobility, and basic bodily functions. The individual is fully dependent on caregivers. End of life may be imminent when the patient starts exhibiting feeding difficulties and increased vulnerability to infections such as pneumonia.
At this point, comfort becomes the central goal. Families may consider palliative or hospice care, which focuses on dignity, pain management, and quality of life. Even if you’re unable to communicate with your loved one, your presence and your touch and soothing audio such as music and nature sounds can be meaningful.
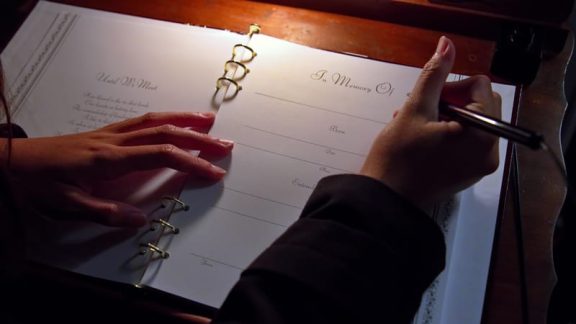
Preparing for and honoring the end of life
Understanding the stages of dementia before death helps caregivers and healthcare teams anticipate the patient’s evolving needs. The progression from mild forgetfulness to full physical dependence highlights the importance of early planning, proactive medical care, and emotional support.
During the final stages and after, caregivers should honor their own grief. Dementia grief can be its own unique experience with predictable challenges – knowing these can help in navigating the feelings.
Dementia changes a person’s abilities but not their humanity. By approaching the disease with preparation, patience, and compassion, families can provide meaningful care through every stage, and honor their loved one’s difficult journey with dignity and grace.